![]() Weather forecasting has saved countless lives over the years, and in Philadelphia meteorologists have taken on an almost mythic status at times, becoming local celebrities. (Thanks, John Bolaris.)
Weather forecasting has saved countless lives over the years, and in Philadelphia meteorologists have taken on an almost mythic status at times, becoming local celebrities. (Thanks, John Bolaris.)
Now there is a new crew on the scene trying to untangle what lies in our future—but they don’t stand in front of green screens or tell you when to bring an umbrella.
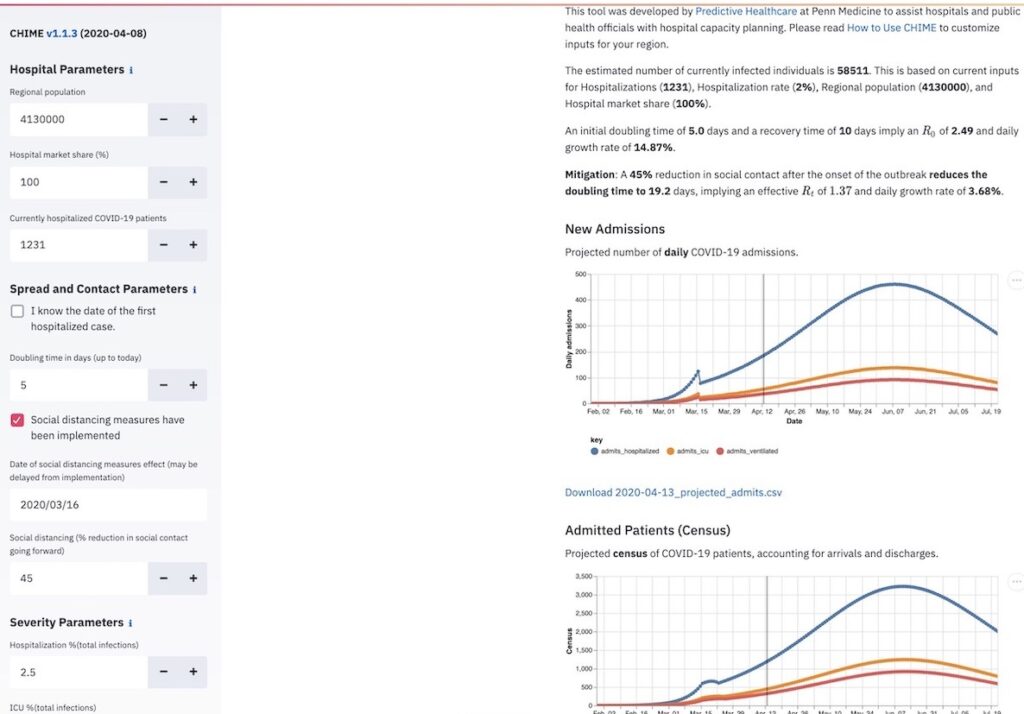
The Predictive Health Care Team at Penn Medicine has built a tool to estimate when Covid-19 hospitalizations will peak, which should help hospital staff plan and prepare. The team’s model, Covid-19 Hospital Impact Model for Epidemics, or CHIME, now predicts a mid-May surge in the Philadelphia region that could overwhelm hospital capacity.
That’s a bit of a contrast with the more highly cited Covid-19 model, developed by the Institute for Health Metrics and Evaluation at the University of Washington.
The IHME model predicts the infections throughout Pennsylvania to peak today, and suggests the state’s hospitals have enough beds to meet the need.
“This is one of a number of publicly available tools for modeling![]() hospital utilization scenarios, each of which can play an important role in helping leaders evaluate and plan for deployment of resources,” Dr. C William Hanson III, the chief medical information officer of Penn Medicine said in a statement. “The purpose of this modeling is not to make predictions with certainty, but instead to provide a range of scenarios which can assist with planning and also demonstrate the effect mitigation efforts like social distancing can have on slowing the spread of the virus.”
hospital utilization scenarios, each of which can play an important role in helping leaders evaluate and plan for deployment of resources,” Dr. C William Hanson III, the chief medical information officer of Penn Medicine said in a statement. “The purpose of this modeling is not to make predictions with certainty, but instead to provide a range of scenarios which can assist with planning and also demonstrate the effect mitigation efforts like social distancing can have on slowing the spread of the virus.”
The CHIME model was developed in-house at the premier research institution, but it has received a lot of help from Philadelphia’s computer programming community, which has helped the online model run faster with more user-friendly features.
Penn Medicine’s Predictive Health Care Team’s modeling now predicts a mid-May surge in the Philadelphia region that could overwhelm hospital capacity.
The Penn Medicine team had just finished a project with Code for Philly to better inform doctors about where they could send patients for medically-assisted treatment of opioid-use disorder.
Michael Becker, a senior data scientist at the Penn Medicine team, got in touch with Code for Philly to help on the new project, working on the biggest public health crisis the planet has seen in a century.
“Even though we’re a big city, it feels like everybody knows everybody, which is how this happened,” says Marieke Jackson, co-director of Code for Philly, which is an all-volunteer group. “The response of people who just want to help and do what they can is incredible.”
The volunteer work on the CHIME computer code has benefitted from the slowdown in most normal business activity, according to Chris Alfano, who helped organize the Code for Philly response.
![]() “Everyone was suddenly home and having trouble working. So we just had this influx of very highly skilled people with a lot of free time on their hands—kinda how we always imagined it where we just write down on the board a bunch of issues and then strangers just show up and know what they’re doing, and fix them on the spot,” says Alfano.
“Everyone was suddenly home and having trouble working. So we just had this influx of very highly skilled people with a lot of free time on their hands—kinda how we always imagined it where we just write down on the board a bunch of issues and then strangers just show up and know what they’re doing, and fix them on the spot,” says Alfano.
Linode, a Philadelphia company, took over the responsibility of hosting the site for free, according to Alfano. (Alfano’s company, Jarvus Innovations, has also done some work for The Citizen)
Programmers are working on another iteration of the CHIME site that will have a new look, according to Alfano, who said there has been some discussion about spinoff projects to look at capacity planning for personal protective equipment.
The utility of the CHIME model is its adaptability. It looks a little clunkier than the IHME, but with just a few data inputs it can make a prediction about the number of people who will be infected, the number hospitalized, and the number in intensive care for any geographic area or hospital catchment at a given time.
Jackson, who has a master’s in epidemiology from New Mexico State University and a full-time job at Health Union, said CHIME uses a “relatively established epidemiological model,” which can quickly spit out results.
Like other models, CHIME creates a bell curve. The worse the conditions are, the taller and thinner the bell.
On its website, CHIME credits Michael Levy, a professor at the Perelman School of Medicine, for his help reviewing the model assumptions, and it also acknowledges Dr. James Lawler, a professor at the University of Nebraska Medical Center, for a late-February webinar about preparing for Covid.
The IHME is easier to use than CHIME, but more limited. The user can quickly pull up the predictions for each state, learning not only about the numbers, but also the specific policies—such as stay-at-home orders that have been put in place.
But state borders aren’t always the best geographic demarcation, especially when dealing with a highly infectious disease.
Philadelphia is located at the southeastern edge of a state that is more than 300 times its size, and Philly has many more connections with parts of New Jersey and Delaware than it does much of Pennsylvania.
Philadelphia Mayor Jim Kenney illustrated this dynamic at a recent press conference, when he said that his mother lives in Jersey, but if she needed to go to a hospital she would go to Jefferson in Philly.
Penn’s CHIME model was developed in-house, but it has received a lot of help from Philadelphia’s computer programming community, which has helped the online model run faster with more user-friendly features.
Officials at the Pennsylvania Department of Health have been consulting the CHIME model, along with one developed by the University of Pittsburgh, and the University of Washington tool, among others.
Vice President Mike Pence said last week that officials are seeing signals that may indicate a forthcoming surge in Philadelphia, and maybe Pittsburgh as well.
At City Hall, Health Commissioner Dr. Thomas Farley sounds more focused on avoiding any bad outcomes than predicting when the local health care system will be under the greatest strain.
“There’s tremendous uncertainty to these models. They predict very different peaks, and different timings of those peaks. We need to be prepared for all of those,” Farley said at a recent press conference. “If we are really successful, we won’t see much of a wave. If we are not successful, we could see a wave that would exceed our hospital capacity.”
But by securing space to treat 200 or more patients at Temple University’s Liacouras Center and trying but failing to use Hahnemann Hospital, city officials have made it clear that they see storm clouds on the horizon, and are making preparations for things to get worse.
Epidemiological predictions are not new, but they have never been attempted at this scale because there has never been a virus outbreak quite like this—at least since the 1918 flu pandemic.
Whereas weather forecasting uses hard metrics like barometric pressure and water temperature, measuring the possible scale and intensity of the Covid-19 outbreak depends in large part on human behavior.
Pretty much everyone has a role to play in determining how many people get sick. In that way, modeling a pandemic may be more akin to making economic forecasts or stock market predictions than charting the likely path of a hurricane.
And of course CHIME might not prove accurate. The CHIME ![]() developers themselves place a big caution atop their webpage warning that there is a “high degree of uncertainty about the details of Covid-19 infection, transmission and the effectiveness of social distancing measures.”
developers themselves place a big caution atop their webpage warning that there is a “high degree of uncertainty about the details of Covid-19 infection, transmission and the effectiveness of social distancing measures.”
The IHME recently adjusted its model to predict 81,766 people in the United States will die of Covid-19 through early August, down from 93,531 just a few days before.
While the science is inexact, it is helpful to have multiple epidemiological studies and models to compare against each other, according to Jackson. Once more data becomes available, more complex models can be built.
Although CHIME was built with hospital and public health officials in mind, anyone with enough knowledge can plug in data to get a hint about how bad it will get, and when things might start getting better.
There is one variable, however, that you won’t find with any precision during the daily briefings on confirmed cases and hospitalizations: the data for the reduction in physical contact going forward, which has enormous bearing on the CHIME forecast.
The CHIME team, who were unavailable for comment, addressed how policies and behaviors to reduce contact could translate into numbers in a blog post, but also acknowledged they made an “educated guess.”
As with so many things in life, we are the ultimate wildcard. We the people, collectively, can help determine if the models were overly pessimistic or not.
Photo courtesy Ryan M. Breeden / Navy Medicine / Flickr