On any given day in Philly, tens of thousands of people struggle with both mental health and substance-use disorder. Often they struggle silently, or in the margins, unable to get care due to financial, social, logistic, medical or other barriers.
During the pandemic and, now, our city’s ongoing unrest, these people—our sisters and brothers, friends and co-workers, neighbors from Kensington to Rittenhouse Square—run the risk of falling further into the shadows.
One group, Pathways to Recovery (PTR), has been providing support to these Get supportDo Something
“Our motto here is really ‘dignity from the door,’” says Denise Botcheos, program director for PTR, the city’s first partial-hospitalization program for addiction treatment and the only one for the dual diagnoses of drug/alcohol and mental health challenges; partial-hospitalization a designation meaning it is the highest level of outpatient care one can receive before in-patient treatment.
For the last four years, the 13-person team at PTR has prided itself on offering nearly 1,000 people six days a week of on-site programming, providing 50 participants at a time up to 45 days of individual, group and family therapy; medication management; transportation assistance; medication-assisted treatment (MAT); psychiatric evaluations; meals; links to housing; case management; and 24/7 on-call crisis support.
In the first half of 2019, 46 percent of PTR participants were able to graduate to a less intense level of care; 11 percent safely transitioned to higher levels of care.
“A huge part of this disease is community. Communities really [are] the largest help for people who are trying to become clean and sober. They need a network, they need support groups, family, friends, a recovery network, their church or synagogue or mosque to help them feel less alone and help them feel strength from others.”
“Isolation for all of us leads to loneliness and boredom, and it’s pushed people who are already residing in unstable or dangerous locations, and who may not have support,” Botcheos says.
How, then, does a program that relies so heavily on in-person gathering pivot during a crisis that has only exacerbated mental health issues?
The short answer: quickly.
They had to pivot immediately.
“Isolation for all of us leads to loneliness and boredom, and it’s pushed people who are already residing in unstable or dangerous locations, and who may not have support,” Botcheos says.
When the shelter-in-place orders went into effect, the team at PTR knew they had to pivot immediately, and realistically: Many of their participants don’t have smartphones, or access to computers, or enough data on their phone plans to support platforms like Zoom, which so many of us have already come to take for granted. So staff members immediately set up Google phone numbers and shared them with participants.
Then, they started holding call-in sessions every day, four times a day.
Charlie, who has struggled with addiction for 20 years (and asked to withhold her name for this article), has participated in other recovery programs over the years. PTR, she says, felt different from the first day; it made her feel like she had a fresh start.
“I’ve learned a lot of things from Pathways. I learned the importance of staying clean one day at a time. I learned positive affirmations, and about consciousness and meditation, which I use for sleeping and for relaxing,” Charlie says by phone one morning from the recovery house where she lives. “They encouraged us to get a sponsor, to work the 12 steps of NA [Narcotics Anonymous], to get numbers from other clients to support each other and to believe in ourselves.”
Now, Charlie attends every single phone session. “To me, the calls are just as powerful. I haven’t missed a beat. We’re still talking about all of the same things that we talked about in-person,” she says.
Support recovery DO MORE
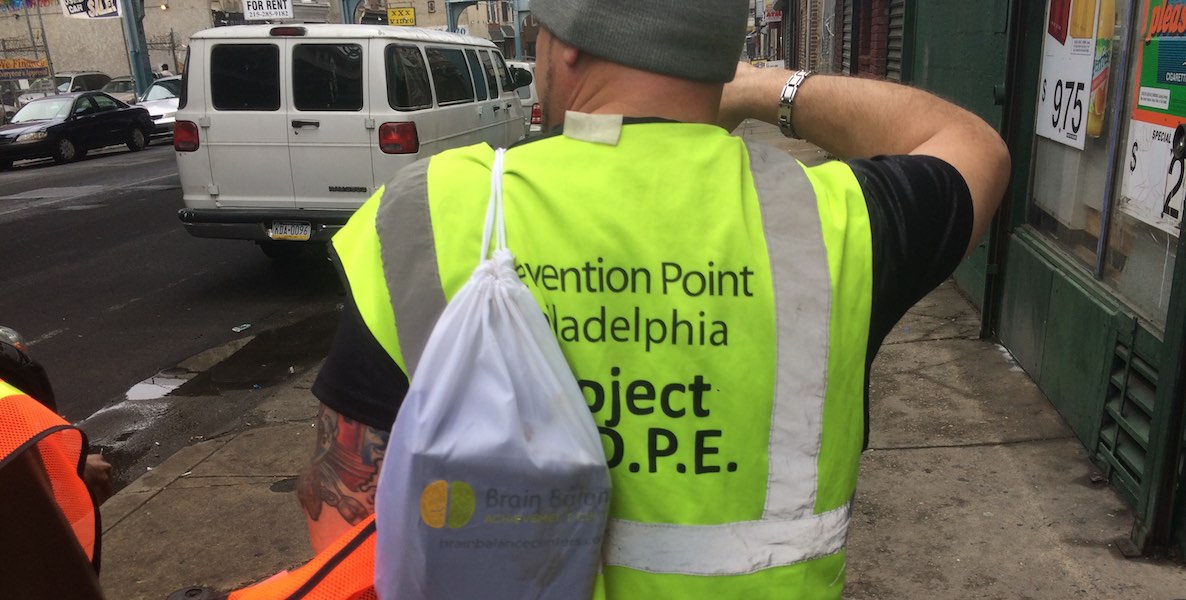
To reach participants they have not heard from via phone or in-person, Peer Recovery Specialist Troy Mouzon has been pounding the pavement: knocking on doors, talking to participants from front stoops or across the street, all while wearing his mask and following all CDC and City guidelines.
A crown jewel among city resources
In Philadelphia, according to 2018 data from the Department of Behavioral Health and Intellectual disAbility Services (DBHIDS), approximately 113,000 Philadelphians received mental health and/or substance use disorder treatment.
Approximately 21,000, or 18 percent, were diagnosed with co-occurring mental health and substance use disorder.
“Addicts won’t always be addicts,” Charlie says. “We do recover. We will survive this.”
Dr. Kristin Van Zant, the medical director of Behavioral Health Services at PTR, says that recovery is different for everyone. “It can be a very nonlinear process. So there’s a step forward. A couple steps sideways. Three steps back. And then a couple steps forward.”
What metrics, then, does the PTR team use to define progress, measure growth?
“We consider it good news when a participant has been with us for seven to eight weeks and gotten stable on psych meds, and stopped or reduced their use of the most lethal or dangerous substances, possibly with the help of Medication Assisted Treatment, [even if] they may not have ceased using every illicit substance,” says Adam Brooks, senior director of addiction services at Public Health Management Corporation (PHMC), the nonprofit public health institute that manages PTR.
Participants typically submit urine samples to guide clinical decision-making and safe prescribing, however urine-testing has been somewhat reduced in light of the pandemic. Brooks refers to PTR as a “crown jewel” among the panoply of City resources, and credits PTR’s devoted staff for the program’s success.
“You have to start from where the person is, and support them each step of the way. And there’s often little pieces that need to be tweaked and supported in that development,” Van Zant says. You have to focus on people’s strengths, not deficits, she says, and give them individualized support.
Right now, that means starting with connection, with reaching out to people who are too often overlooked in our city, and in cities nationwide.
“Just today, two people were telling me how hard it is to feel completely alone, to Addiction in PhillyRead More
Still, while the pandemic and protests may present myriad new hurdles, they haven’t caused Charlie, like many of her PTR peers, to waver from a belief she holds dear, a belief that motivates her, and one that she wishes others would heed as well:
“Addicts won’t always be addicts,” she says. “We do recover. And there’s a lot more to us than the drugs that we used. We are still human beings. We reach for a higher goal if given the higher opportunity and the chance. We will survive this.”
Photo courtesy Toimetaja Tõlkebüroo / Unsplash