On a Sunday in early February, Reverend Doctor William J. Shaw took the pulpit in front of rows of empty pews at White Rock Baptist Church in West Philadelphia. Hundreds of congregants tuned in on Facebook Live. Before starting his sermon, he did what many pastors in West Philly did that morning: announced a new opportunity to get vaccinated.
“It’s well known that where the vaccines have been provided, members of minority communities have received fewer inoculations compared to members of other ethnic communities,” Shaw went on. “Our communities have been victims of so many reasons why we haven’t done so, why we can’t do so—we’re attempting to overcome some of those barriers.”
The comments rolled in on Facebook. Thank you for ensuring our senior community gets educated, informed and vaccinated, one said.
The pastor continued. “I must express my own irritation, my own agitation, over the structural barriers that have existed before now in receiving health care… But even with that, I would ask that you share in this effort. We will help you do it… Blessings be upon you.”
The following Saturday, Reverend Shaw was the first to get vaccinated, followed by other pastors, then members of their congregations. More than 500 West Philadelphians, 95 percent of whom were Black, got a shot that day—the first community clinic of the #VaccineCollaborative organized by the University of Pennsylvania Health System, what was then Mercy Catholic Medical Center and faith leaders from throughout West Philly.
“It’s going to where it’s needed. If you want to address population health, I think this is a start,” says Penn’s Nida Al-Ramahi.
From mid-February through mid-April, they held six clinics in West and Southwest Philly, fully vaccinating 2,821 Philadelphians, 85 percent of them Black. They did it by harnessing the power of their faith communities, led by trusted leaders whose word held sway among even reluctant congregants, and designing the clinic with the Philadelphians they sought to serve—those who experienced the worst impacts of the pandemic and had less access to the vaccine.
Though the number vaccinated through the collaborative is small, the lessons learned could go well beyond vaccines, or even Covid-19.
“[The #VaccineCollaborative], in a way, is at the pinnacle of moving towards a reimagined healthcare delivery model,” says Penn Health Director of Strategic Operations Nida Al-Ramahi. “It’s going to where it’s needed. If you want to address population health, I think this is a start.”
“What Can We Do?”
Nationally, adjusted for age, Black Americans have been 2.8 times more likely to be hospitalized and two times more likely to die of Covid-19 than white Americans. Of the 17,025 (reported) Philadelphians who were hospitalized due to Covid-19, half were Black and just 20 percent were white (those groups each make up a little more than 40 percent of our city’s population).
And once vaccines became available this year, the numbers were similarly uneven: As of June 14, across the 43 states reporting demographic vaccination data, white Americans have received vaccines at rates 1.4 times higher than Black Americans.
Here in Philly, since doses were first available in the city late December up until mid-April, white residents were vaccinated at about twice the rate of Black Philadelphians. Just in the past two months, the gap has narrowed slightly. As of June 27th, 52 percent of white Philadelphians and 33 percent of Black Philadelphians have been vaccinated.
The problem surfaced at Penn, which struggled to vaccinate its own Black staff members at the same rate as white workers—an issue addressed in January, when Dr. Florencia Polite and Aron Berman worked with other institution leaders to launch Project CAVEAT, a messaging program to encourage Black staffers to get their shots.

At the same time, Penn Medicine Chief Operating Officer Phil Okala knew that many of those same staff members were part of the West Philadelphia communities that faced the most barriers to vaccine access—including inconvenient locations of clinics; web-based scheduling requiring WiFi, dedicated time and tech-savviness; plus skepticism earned by a long legacy of racism in healthcare.
“When we knew that we had to do something outside of our four walls of Penn Medicine—engage the community directly—I called [Reverend Shaw],” Okala says. As so many cities across the U.S. have learned (or not), trusted messengers are key in instilling vaccine confidence. “The tactic of reaching out to faith leaders was to try and make sure that we leverage what is historically an influential institution in the African-American community.”
Shaw, who recently marked 65 years leading White Rock Baptist Church, had spent the pandemic pastoring to his parishioners via the Internet, preaching on Sundays, facilitating virtual funerals for those who died of Covid-19, holding hands (virtually) with a community that was devastated by the pandemic. And as chair of the board for the Hospital of the University of Pennsylvania, he’d leaned on the institution for data on how the virus was impacting his community.
In January, Shaw helped bring 20 pastors of Black churches in West and Southwest Philly to join a call with Okala and Dr. P.J. Brennan, Penn Medicine’s chief medical officer, about how they could help bridge the vaccine racial gap. First, though, many of the pastors had their own questions about the vaccine, which Dr. Brennan, an infectious disease expert, spent a good portion of the call answering.
Then, Okala posed the question, What can we do?
One pastor suggested what he felt would move the needle: vaccinating the pastors. If people could see their own leadership receiving the vaccine, they’d feel more confident in signing up for the shot themselves.
Okala and Brennan took the idea back to their team. “We discussed it internally, and thought, Why not even make this bigger?” Okala says. “Why just do the pastors? How about having a vaccine clinic?”
Designed with Intention
That idea required a rethinking of the way Penn and other hospitals have traditionally doled out medicine—something Penn Medicine CEO Kevin Mahoney has declared part of the institution’s mission (and which sped up during the pandemic). For example, Penn has partnered with WURD Radio and the Independence Blue Cross Foundation to mail out screening kits for colorectal cancer—which Black adults are 40 percent more likely to die from than white adults—and then absorb the cost of the workup if a person doesn’t have insurance.
There’s the myriad research and training happening at Penn’s Center for Health Equity Advancement, and the new policy that ties Penn Medicine’s executive pay directly to hospitals’ reducing morbidity and mortality rates among Black and brown patients.
But Okala and the others realized that to really reach the residents who were hesitant, couldn’t make vaccine appointments, or couldn’t get to far-away clinics, they’d need a more grassroots approach to community engagement and education from trusted messengers, and health care providers of and from the community.
“I and many other Black physicians have unique insights and understanding of the historical and ongoing way that racism impacts or manifests within our institution,” South says, “and also what’s happening in the community and the structural barriers that are patterned by race in this country that shape neighborhoods, that shape the distribution of resources.”
For that, Okala and the others turned to Mercy Catholic Medical Center Philadelphia, a community teaching hospital that has provided care for primarily low-income West Philadelphians for more than 100 years. (This spring Penn partnered with Public Health Management Corporation and Independence Blue Cross to take over Mercy to keep it from closing.)
Mercy, whose leaders were also seeing a vaccine disparity, already had relationships with many faith leaders in West Philly, including Reverend W. Lonnie Herndon, who leads the Church of Christian Compassion, one of the largest Black churches in West Philadelphia, with about 5,500 congregants. After speaking to Rev. Shaw, Herndon offered his church for the first clinic, scheduled for just two weeks later.
 Penn brought in Project CAVEAT’s Dr. South, assistant professor of emergency medicine and faculty director of the Urban Health Lab, to act as a liaison between the hospital and the community. South says that for her work on the community clinic, her lived experience as a Black person was even more crucial than her professional experience.
Penn brought in Project CAVEAT’s Dr. South, assistant professor of emergency medicine and faculty director of the Urban Health Lab, to act as a liaison between the hospital and the community. South says that for her work on the community clinic, her lived experience as a Black person was even more crucial than her professional experience.
“I and many other Black physicians have unique insights and understanding of the historical and ongoing way that racism impacts or manifests within our institution,” she says, “and also what’s happening in the community and the structural barriers that are patterned by race in this country that shape neighborhoods, that shape the distribution of resources.”
She helped lead virtual vaccine education events with the pastors and congregants, and ensured that the community leaders informed the design of the initiative at every step.
For example, church leaders insisted that their congregants needed to be able to sign up for appointments by phone—not just by text, as first proposed—and that one person could help sign up multiple people. “Some of our members still have rotary dial phones,” says Lavonia Moore-Washington, White Rock’s office manager and Reverend Shaw’s personal assistant.
To sign up, congregants, or someone on their behalf, could call and through IVR (interactive voice recording) use their keypad to get signed up without waiting on hold. Or they could text the word “Ready,” and then submit the information needed and schedule an appointment via text. People could register any time of day in a matter of minutes, even if they didn’t have access to the internet.
That seemingly small change—driven by community members’ insights—paid off; 37 percent of post-vaccination survey respondents cited ease of sign up as a factor in deciding to get vaccinated.
“I know I’m okay because you’re here.”
After the first successful #VaccinationCollaborative clinic at Christian Compassion, the team reached out to other community leaders—barbershop and salon owners, senior centers, RCOs, committee people—to get the word out about the next vaccination events.
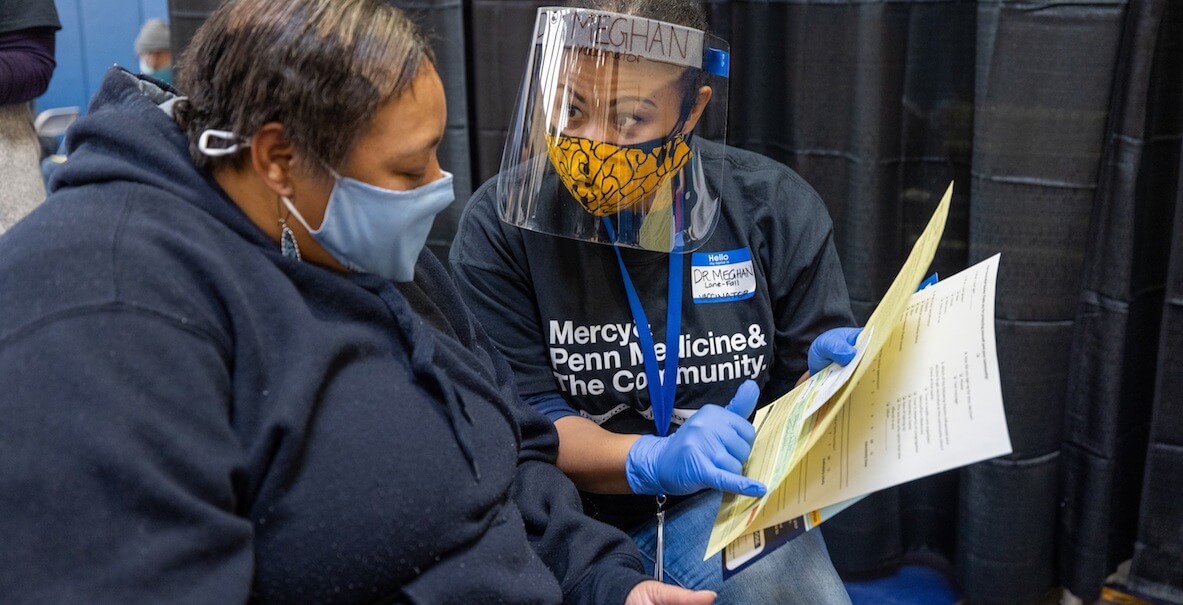
Dr. Chidinma Nwakanma, emergency doctor at Penn Medicine and one of the lead physicians on the collaboration, joined WURD for a segment to spread the word about the opportunity and debunk common myths about the vaccine. She talked about the importance of having Black medical professionals working at the clinics.
“This past week it was myself, another Black physician and a Black pharmacist,” Nwakanma told WURD. “And the amount of people that came up to us and said, I know I’m okay because you’re here, or, Thank you for taking care of us, or I was nervous before but now that I see it’s you I feel more at ease about getting this. That means everything to me.”
Indeed, 56 percent of survey respondents reported that their trust in healthcare organizers was a factor in deciding to get vaccinated. (Many even brought gifts to the clinicians when they returned for their second shot.)
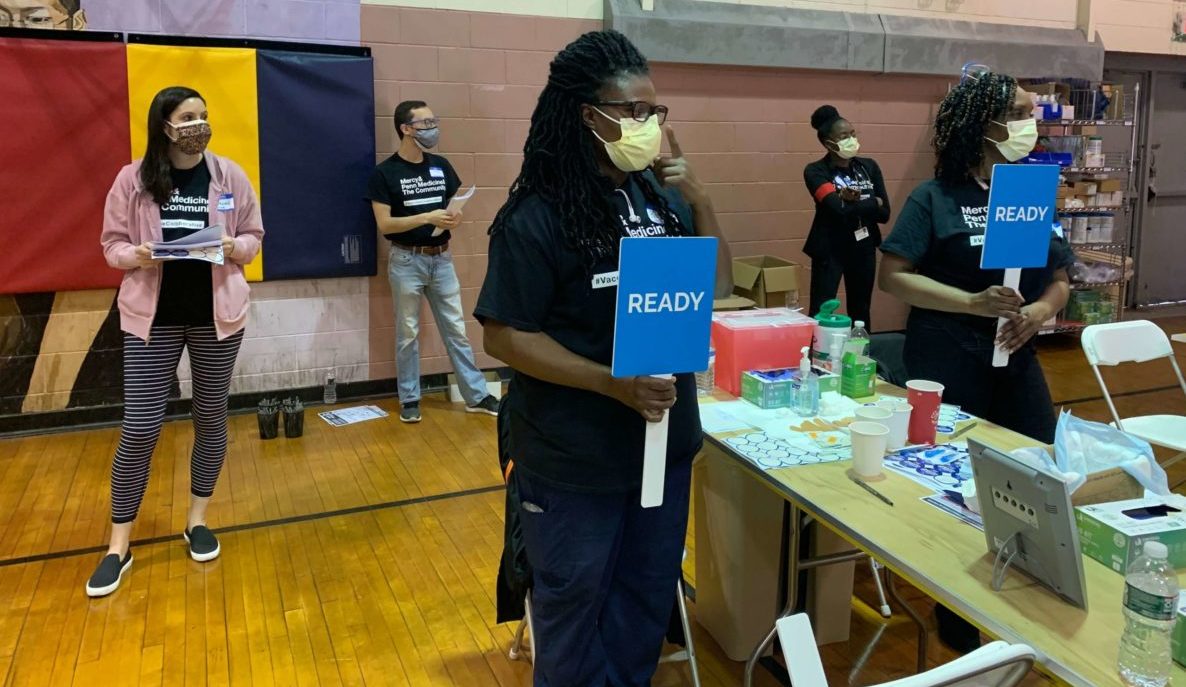
At the fifth vaccine clinic, held in the gym at the Francis Meyers Rec Center in Kingsessing on a Saturday in late March, the vibe was relaxed, hushed except for the hum of a generator. There was no line, just intermittent entry and exit at the front door—volunteers stood at tables, receiving folks to check in. Another group escorted people from check-in to the clinicians who held up blue paddles displaying the word “ready” under the basketball hoops. After the shot, more volunteers walked patients to the folding chairs lined up across the court.
“There was a very high level of face to face interaction,” says Roy Rosin, chief innovation officer at Penn’s Center for Healthcare Innovation. His colleagues Dr. Kat Lee, Lauren Hahn and Nida Al-Ramahi led the design of the clinics themselves—another rethinking of the norm. “The team did a fantastic job making sure everyone felt like they belonged and making sure there wasn’t going to be a moment of doubt or uncertainty about how it was going to work.”
During the consent process, for example, instead of simply handing individuals a piece of paper to sign, they gathered six to eight people at a time to provide education and answer questions as a group. It made the nerve-wracking process of signing that you understand the benefits and risks of vaccination and voluntarily assume full responsibility for any reactions that may result a bit less scary. And it was efficient. Clinicians didn’t feel pressured to rush through—they could take time and leverage folks’ questions so that everybody left with a better understanding of how the vaccine works and its risks and benefits.
“We didn’t want to leave anyone hanging, so they got follow-up guidance about what they might be feeling over the next few days,” says Hahn. Attendees were also given a phone number they could call 24/7 in case they didn’t have a primary care doctor. “We’ve borrowed from so many different redesign projects that have happened in outpatient, inpatient and ER care,” says Lee. “We learned from models that work and are inclusive.”
“What are your goals and what scares you?”
More than just protecting vulnerable Philadelphians from Covid-19, the #VaccineCollaborative model provided a model for bringing quality healthcare to vulnerable populations in every neighborhood. One way is by literally offering more primary care and family medicine in every neighborhood. “Typically we operate in a traditional setting of what we think healthcare should be, which is physically going to a hospital or to a doctor’s office,” Al-Ramahi says. “Making sure that we meet people where they are is so critical in making it a very patient-centered type of care delivery.”
According to a 2016 study on Philly neighborhoods, the odds of having low-access to health care—defined by travel time—were 28 times greater for census tracts with a high proportion of African Americans than in tracts with a low proportion of African Americans. Actually decreasing the travel time required for underserved populations to get care would make a huge impact.
“If you get into those questions, What are your goals and what scares you? I think you can design care in a more human and more effective way,” Rosin says. “You will help people understand that you actually care about them—and then you have the right to care for them.”
And, as Rosin points out, the #VaccineCollaborative showed that it’s also important to “meet people where they are” technologically and emotionally—not just physically. “Technology is neither ‘good’ nor ‘bad,’” says Rosin, citing a common debate in healthcare. “But the choice of the technology is critical.” In this case, efficient, scalable and high tech on the backend, but low tech, human and accessible on the patient facing side was key.
Emotionally, it’s about asking different questions—and listening. “If you get into those questions, What are your goals and what scares you? I think you can design care in a more human and more effective way,” Rosin says. “You will help people understand that you actually care about them—and then you have the right to care for them.”
It’s possible to scale that idea beyond the individual level by ensuring members of the communities we’re seeking to serve are at the table—as regular members of the dinner club, not just special guests. Dr. South sees a future where Penn Medicine hires community members to serve in advisory roles within each clinical department and executive offices, to help inform the needs of those it serves. “Community members should be at most leadership meetings and giving input and insight into decisions that affect the health and wellbeing of the community as those decisions are being made,” she says.
That could start, she says, with existing staff members who live in West and Southwest Philadelphia, who in turn could benefit from the professional development that inevitably comes with proximity to power. “Why not have them work one less shift per month and instead use that time to work with leadership?”
Rosin thinks the first step towards making changes like these on a broader scale is distilling learnings from the #VaccineCollaborative into principles and communicate those widely. Then, incentivize the desired outcome without being overly prescriptive.
He threw out, in his words, a “crazy” example. “Let’s say you think meeting people where they are geographically matters. Maybe a metric is travel time for people in certain zip codes to access care. You might create a city dashboard that publicly tracks this metric, visible and tangible awards and recognition for organizations that impact it positively, and even financial incentives aligned with interventions that achieve a certain standard.”
Crazy? Or could it be just the type of fresh thinking and pragmatic incentivizing we need to truly make change?
The Citizen is one of 20 news organizations producing Broke in Philly, a collaborative reporting project on solutions to poverty and the city’s push towards economic justice. Follow the project on Twitter @BrokeInPhilly.
Header photo courtesy of Penn Medicine