“It was a night shift that I was staffing, and a young man walked in and he had a friend with him,” recalls Dr. Theodore Corbin, an emergency room doctor at Hahnemann University Hospital. “The friend was pulling him in — walking him, and the gentleman who was going to be a patient had his shirt off. And then it looked like there was a piece of plastic-wrap that was across his stomach. The piece of plastic-wrap was his intestines; he had been stabbed.”

According to Census Data, 1.5 million people are treated annually in a U.S. emergency room for violence-related injuries. Within five years of being discharged from the hospital, 45 percent of severely wounded victims will be re-injured; and close to 20 percent will be dead—that’s 300,000 who do not survive a second violent encounter.
These emergency room patients are suffering from more than just physical trauma. Devastated psychologically, they are caught in a cycle of violence largely ignored by the medical and justice systems. Discharged from the hospital, they are left alone to deal with the aftermath of disaster.
That’s why Corbin, himself born and raised in Philadelphia, designed Healing Hurt People—now in five local emergency rooms—to address the gap between the physical and the psychological treatment of victims of violence.
As an emergency doctor for nearly a decade, Corbin has observed a high number of victims of intentional injury. “When I first started doing emergency medicine I would do around four shifts a week,” he says. “And in every single shift I would see someone who was impacted by violence.”
He also noticed how the victims of these situations were neglected after they had been discharged from the hospital. More important, he noted how the hospital did not address the trauma suffered by patients, their families or friends.
It was the stabbing incident that sparked the search for a solution. Corbin describes what happened later that night. “We got him into the trauma bay, we called the trauma team and he lived and he was fine, but the thing that I thought so profound was the young man that brought him in” Corbin says. “I said, ‘Is he related to you?’ He said, ‘No’. I said, ‘Are you okay?’ He said, ‘I don’t know’. And in that moment I thought: There are a lot of these situations, there are a lot of people that see these things happen, and there is essentially nothing to help him with what he has just seen.”
Corbin, now an Associate Professor in Drexel’s Department of Emergency Medicine and co-director of The Center for Nonviolence & Social Justice, set about pulling together a team of professionals, including an emergency physician, a psychiatrist, an internist, a social worker and a psychologist knowledgeable in violence prevention and trauma. Together, they devised a plan. They called it Healing Hurt People (HHP) and they started seeing patients at Drexel-Hahnemann in 2008.
HHP’s goal is to improve the lives of victims in the aftermath of a violent encounter by treating the psychological trauma suffered by not only the victim but, in some instances, their family and friends as well. In the fall of 2009, HHP was expanded to St. Christopher’s Hospital for Children to reach young victims of violence, ages eight to 21. Now it also operates at Einstein, Penn Presbyterian and Temple emergency rooms.
Since it started, HPP has worked with 1,800 victims and even more families, and the model has been replicated in Chicago and Portland, Oregon. This spring, HPP won an award from the Office for Victims of Crime, a division of the Justice Department.
HHP begins as soon as the victim has been medically stabilized, and continues for up to a year. During a hospital visit, an HHP social worker educates the patient about the possible mental and psychological effects of what they’ve been through. They also make sure that the client has a safe place to go when they’re discharged; if their own homes are not safe enough, they will be taken to a shelter or a relative’s home.
Corbin believes that some practices imposed on people of color have made them wary of acknowledging certain feelings, bringing them out, talking about them. Corbin, who is African American, is no exception to these forces. “I feel like I’m contributing to society, and yet I still experience micro-aggressions,” he says.
This initial introduction is followed by the home-visit phase, with the client being seen at home, coming in to HHP offices, or meeting in a mutual location. The social worker will observe the client’s living situation and try to remedy any collateral issues—the client’s educational history, health history, involvement, if any, with the criminal justice system. The social worker will also ask the client about their life goals and how HHP can help them achieve them. For a period of six months up to a year, HHP staff occasionally engages with the client’s family who, most of the time, are also traumatized.
![]()
The program infuses all of this with counseling and coaching. “Social workers are trained in brief supportive counseling, collateral therapy, trauma therapy, different modalities to help the person heal physically and emotionally,” Corbin says. Clients also get one-on-one mentoring and participate in peer support groups to talk about trauma.
In the core of the city, interpersonal violence largely affects people of color, particularly males between 15 and 29—some 75 percent of shooting victims in the city are under the age of 34—who are often affected by issues of racism, rejection, social inequality and injustice. Corbin believes that some practices imposed on people of color have made them wary of acknowledging certain feelings, bringing them out, talking about them. Corbin, who is African American, is no exception to these forces.
“I feel like I’m contributing to society, and yet I still experience micro-aggressions,” he says. “If I didn’t have an understanding or a framework, I would be an angry person wanting to get revenge in some capacity.”
Within five years of being discharged from the hospital, 45 percent of severely wounded victims will be re-injured; and close to 20 percent will be dead—that’s 300,000 who do not survive a second violent encounter.
Corbin was recently awarded a fellowship by the Stoneleigh Foundation—which funds people working towards social change—and is conducting a study on the long-term effects of the HHP model, to satisfy the need for an evidence-based practice and to qualify for additional funding. But he emphasizes that he doesn’t believe in counting only the positive outcomes. He feels that anyone touched by HHP has something more than they had before they encountered it.
![]()
“Anyone that comes into contact with any of our providers, social workers or intervention peer specialists is going to receive some basic psychoeducation,” Corbin says. “For example, just the acknowledgement that what you have been through is terrible; suggesting that here are some feelings that you might want to be aware of that you might experience. At the very least that’s what anyone is going to get and I would say that’s a win in terms of us being able to give some people some language about what they are experiencing.”
The group has had some remarkable successes. Two young men who went through the program are now HHP staff members, working in the ERs at Hahnemann and St. Chris. “They have done their work in terms of their physical and emotional healing,” Corbin says. “Now they staff the emergency departments on the weekends on the peak hours when a lot of intentional injury happens, to impart psychoeducation and the necessary support for the families and the patients that have experienced that violent encounter.”
![]() Still, Corbin concedes that the HHP team has also had some failures, particularly with clients who did not keep consistent contact with the social workers. In one case, that failure led to a client dying from gun violence. HHP only works with those who are ready to let go of the part of their life that led them to the hospital in the first place.
Still, Corbin concedes that the HHP team has also had some failures, particularly with clients who did not keep consistent contact with the social workers. In one case, that failure led to a client dying from gun violence. HHP only works with those who are ready to let go of the part of their life that led them to the hospital in the first place.
“They are lying in a gurney in a hospital and they say to themselves, ‘I have to do something different,’” Corbin explains. “These people are ripe for Healing Hurt People services that will help them change their trajectory, and the social worker walks into their lives and their journey to healing begins.”
That journey centers around the idea of “SELF”, which the social worker addresses with each client:
- Safety: what the client’s idea of safety is and what can be done to make them feel safer. In some instances, it might mean moving them to a new school or into a new neighborhood.
- Emotional Management: how the client manages negative feelings of revenge, micro-aggression and other forces that might be oppressing them.
- Loss and Letting Go: what or who a client needs to let go of to make changes, and how letting go is going to affect them emotionally.
- “Future:” where the clients would like to see themselves in the coming years. Corbin says that it is hard for most clients to envision themselves beyond the Philadelphia area. Most of their dreams are contained within the walls of this city, which demonstrates the challenge of poverty and lack of access. The clients do not know of the opportunities that lie beyond Philadelphia. Furthermore, the victims’ futures are affected by the past—early experiences have a long-term effect on the individual.
Corbin’s ultimate goal is to develop standards for any hospital that experiences a large volume of intentionally injured individuals. How he’ll expand HHP depends on the results of the long-term study. He expects his research will prove what he’s seen all along—that HHP works—and that he’ll be able to raise money to expand and implement the program in more hospitals—so he can heal more hurt people.
Lebo Ashley Phillip is a student at the University of Botswana who reported this story on her school term abroad at the University of Pennsylvania. A version of it originally appeared on SafeKidsStories. It’s the first of series of articles that will run on both sites.
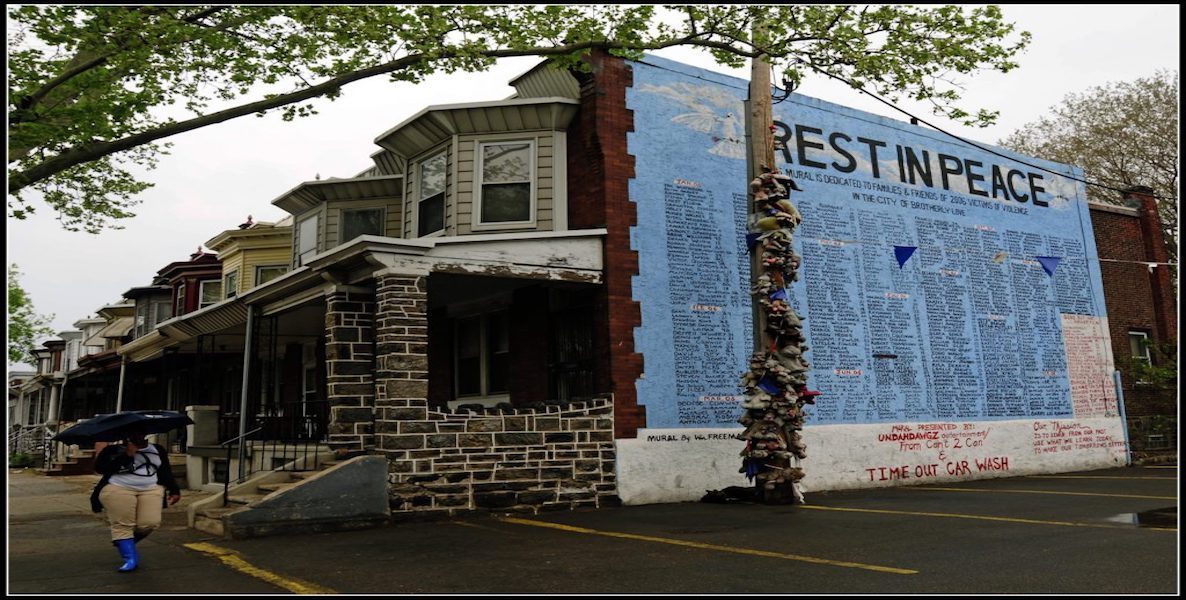
Header Photo: Flikr