The year was 2016 and Oklahoma, like the rest of the country, was experiencing a mental health crisis.
Josh Cantwell, COO of the nonprofit GRAND Mental Health, which has been serving Northeast and North Central Oklahoma since 1979, vividly remembers the behavioral health landscape at that time: Too many citizens were in crisis. Too many were suicidal.
And police officers were investing far too much time — and money — responding to situations that were better suited to health care professionals. They were spending hours waiting in emergency departments and driving around the state to get folks from evaluations in one hospital to treatment in another. In rural communities where only a handful of officers worked any given shift, these cases were keeping officers from supporting other critical local needs.
It was an issue of public safety, public health, efficiency, and economy.
Cantwell’s colleague, GRAND CEO Larry Smith, saw the need for alternatives to the existing resources — the emergency department and inpatient mental health care hospitals. As timing would have it, it was also around this time that the federal government invited mental health care providers to participate in the Certified Community Behavioral Health Clinics (CCBHC) demonstration model program, an initiative that, in a nutshell, incentivizes mental health and substance abuse treatment providers with increased federal funding for demonstrating positive, data-backed outcomes for patients. (For more on the origin and national rollout of CCBHCs, read this excellent New York Times piece).
“Everybody who works for us is making enough money to take care of their families. They can be proud of the job that they have, says Josh Cantwell. “They see advancement opportunities. They see a field that’s now respected. There’s a real shift.”
And so Smith and Cantwell (himself a licensed clinical social worker and certified peer recovery support specialist), and their team stepped back and asked themselves: In an ideal scenario, what could additional funding help us achieve?
In response, the team developed the GRAND Model, which has three parts:
-
- It introduced Urgent Recovery Centers (URCs) to provide 24/7 crisis stabilization services that were far less intensive and resource-draining than inpatient treatment.
- It began distributing iPads to GRAND patients, first responders, hospitals, and community partners to provide instant access to a GRAND mental health provider anytime, anywhere.
- And — critically — it ensured that all iPad and crisis calls would be answered by fully trained, engaged, and on-duty clinicians who’d be onsite at a URC.
Since introducing the model, outcomes have been staggering: Inpatient hospitalizations among GRAND adult clients at any Oklahoma psychiatric hospital were reduced by 93.1 percent. From 2016 to 2021, this reduction saved more than $62 million. The number of adult clients served increased by 163.5 percent. And law enforcement in seven counties saved both 576 days in time spent transporting clients and over $718,000 from reductions in time and distance spent transporting clients.
What has transpired in Oklahoma has been nothing short of transformative — and holds lessons that healthcare providers, policy makers, law enforcement agencies, investors, and mission-driven technologists in Philadelphia — where just over 20 percent of adults have a mental health diagnosis and, between November 2020 and October 2021 alone, police identified 55,000 of nearly 2.4 million calls as requiring crisis intervention — would be wise to heed.
“URCs” as alternatives to the emergency department
No one would argue that it’s a giant waste of a law enforcement officer’s time and training to spend hours waiting in an emergency department (ED) for a physician — whose expertise is not psychiatric evaluations, anyway — to diagnose a client. It becomes an even bigger waste of resources when options for that client, once evaluated, are essentially limited to inpatient hospitalization at a mental health care facility.
Recognizing this, GRAND launched a series of Urgent Recovery Centers, alternatives to the Emergency Department or inpatient hospitalization for mental health emergencies. URCs accept both walk-ins, and drop-offs from law enforcement.
GRAND’s first URC, in the northeastern corner of the state, was configured as a large room with plexiglass walls that’s staffed by trained clinicians: a licensed mental health professional, a registered nurse, and two recovery support specialists. It was designed without beds, but with reclining, comfortable chairs.
“The same people who are talking to the individuals on the street are the same treatment providers they’re going to meet once they get to the facility.” It’s not someone who’s on call. “They’re awake, they’re alert, they’re ready to intervene, and they’re ready to help law enforcement officers 24/7,” says Josh Cantwell.
The idea was for it to become a centrally located place within the community where police officers could bring in a client who seems to need mental health care, but doesn’t necessarily need the intensive care of an ED or inpatient hospital — like someone experiencing psychosis, or someone at risk of harming themself or others. Law enforcement could then leave the client in the safe care of the URC staff, and return to their regular shift duties — saving hours, dollars and resources.
“Because of the [plexi]glass design, workers had a line of sight from everywhere, so we could safely do more with our staffing pattern,” Cantwell explains. “With no beds and nobody staying the night, there was no need for private rooms either.”
After the first center opened, mental health recidivism — specifically psychiatric inpatient hospitalization — went down, the Oklahoma Department of Corrections saw fewer people, and clients saw improvements to their mental health. Now, GRAND oversees three URCs. With 24 staffers split between the three facilities, they have a capacity of 75. Four more URCs are scheduled to open around the state in 2023.
Tech for good: iPads as an extension of care
In conjunction with the URCs, GRAND also began to distribute specially-outfitted iPads to a small group of community partners — law enforcement and hospitals, high-risk clients discharging from the URC, and GRAND therapists and staff. GRAND covers the cost of the devices’ data plans.
Each iPad has a large crisis button that connects to a GRAND therapist any time of the day. It also has functions that track, monitor, and coordinate care needs, appointments, and outcomes. Staff can also use the tablet to see medications and a client “report card” that tracks progress towards goals — a key feature when measuring and reporting outcomes. (These are not fully loaded iPads — they are single-function devices, loaded only with the GRAND tools.)
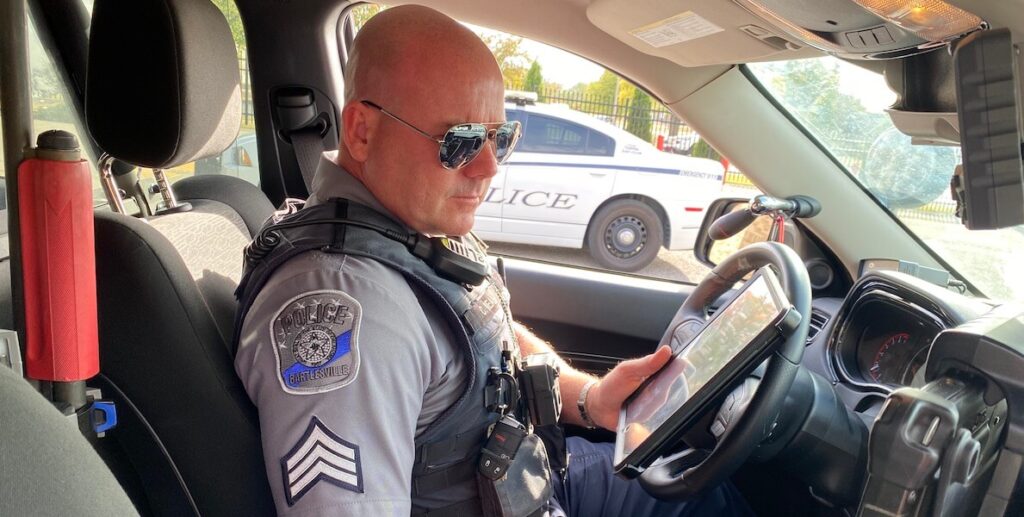
Police officers use their iPads to consult with therapists when they are out on a call, for crisis intervention and stabilization, and referrals. The tablet allows the therapist to be present for a virtual assessment, without needing to ride along with the officer or meet them on-site — which eliminates safety, logistical, liability, and cost concerns.
“We are not afraid to stop something dead in our tracks and shift gears. We’re not married to any idea. If it’s not working, we’re going to fix it,” says Josh Cantwell.
Since the GRAND Model has been implemented, GRAND has also given devices to college campuses, museums, libraries, churches, and other community sites, where managers have access to them any time there’s a situation that they believe warrants support. Now, there are 9,591 iPads in circulation with patients, and another 1,786 with first responders. (Cantwell says GRAND hovers at just below a 10 percent loss rate for the devices, a figure he’s tried mightily to improve but concedes he may just have to accept as a cost of doing business.)
24/7, 365 responses
It’s not enough to just hand out iPads: For any mobile technology crisis response program to work, the crisis button calls have to be immediately answered every single time, and provide tangible help. In the GRAND model, calls are answered by clinicians who are awake and working at the URC. The goal is to have all calls answered within one to three rings; calls first ring to therapists, then a trained Recovery Support Specialist, with nurses and the unit coordinator as the last tier.
“The only thing worse than somebody not having access to this is them thinking they have access, and it not working,” says Cantwell. GRAND’s 22 staff members who answer iPads do other jobs as well. “That’s how we afford it — that’s not all they do,” Cantwell says. “The same people who are talking to the individuals on the street are the same treatment providers they’re going to meet once they get to the facility.” It’s not someone who’s on call. “They’re awake, they’re alert, they’re ready to intervene, and they’re ready to help law enforcement officers 24/7,” Cantwell says.
Maximizing the federal CCBHC model
To be clear, none of the progress Oklahoma has made would be possible without the CCBHC demonstration model framework. CCBHC demonstration model funding and its focus on measurable, data-backed outcomes has been critical — not just for funding for tools like iPads and the creation of the URCs, but to be able to pay employees a livable wage — something that’s too often uncommon in the behavioral healthcare space.
“I used to sit around in meetings and someone would invariably say, Well, we didn’t go into this for the money, haha – and everybody would laugh. And I always thought, Well that’s why we’re not getting outcomes!” says Cantwell.
Now, GRAND is paying staff enough to attract talent from around the country. “Everybody who works for us is making enough money to take care of their families. They can be proud of the job that they have. They see advancement opportunities. They see a field that’s now respected. There’s a real shift,” Cantwell says.
“I think about how Pennsylvania is the exception,” Richard Edley says. “Why do we always have to be so special?”
GRAND has also created an extensive curriculum to onboard and train staff, a program that goes beyond traditional compliance modules. To maximize human resources, GRAND has also created a unique role — the “ITM,” or integrated team manager — who spearheads a patient’s care, thus freeing up physicians’ time spent dealing with administrative tasks, and maximizing the amount of time clinicians can instead spend with patients.
What’s more, GRAND is working with the Israel-based company ELEOS to introduce an augmented intelligence program that takes accurate, live notes during sessions — a task that has notoriously fueled burnout and thwarted productivity among healthcare providers.
Another ingredient in Oklahoma’s secret sauce: collaboration across the state. Cantwell says that none of the progress his team has seen would have been possible without the support of and collaboration between Carrie Slatton-Hodges, Commissioner for the Oklahoma Department of Mental Health and Substance Abuse Services, Larry Smith, and state Medicaid and Medicare agencies.
Most of all, GRAND is committed to continually thinking outside the box: “We are not afraid to stop something dead in our tracks and shift gears. We’re not married to any idea. If it’s not working, we’re going to fix it and we’re going to do CQI [continuous quality improvement] on the process until we fix it,” Cantwell says.
That philosophy is at the heart of another creative solution GRAND is rolling out this month: a brief-stay therapeutic home. It will be a fully video- and microphone-connected home with a control center in the garage, where families in crisis live for five days at a time, being observed and guided by professionals through the challenging dynamics their family is experiencing. It comes in response to the alarming number of kids going into inpatient hospitalization and the foster care system.
Why does Philly have to be special?
Oklahoma and Philadelphia are not an apples-to-apples comparison. But there are decidedly replicable, scalable take-aways to be had. So what’s holding back Philly at a time when violence is up, the police force staff is down, and our communities are desperate for mental health support?
Well, Pennsylvania was initially part of the CCBHC demonstration model program. But in 2019, the Commonwealth decided to pull out of the program. A rep from the PA Department of Human Services explains: “We made the decision to exit the demonstration in 2019 when its future federal funding was unclear.”
Instead, the Commonwealth created its own homegrown version of the program, Integrated Care and Wellness Clinics (or ICWC, called “ICK-wick”); Philadelphia was required to follow suit. According, again, to the Department of Human Services: “The ICWCs provide the same nine core services but were designed to be financially sustainable should the federal funding have been discontinued. We continue to evaluate future opportunities and continue to work with our federal partners at CMS/SAMHSA to maximize resources for behavioral health programs in Pennsylvania.”
But some experts believe PA’s decision was short-sighted. “We always thought it was a very quick trigger on what could’ve been a great program,” says Richard Edley, PhD, the president and CEO of RCPA, one of the nation’s largest health and human services trade associations. “It was just in an early pilot stage. They could have worked with the feds and Centers for Medicare & Medicaid Services to improve the process over time.”
Plus, as demanding as the CCBHC reporting requirements are, they serve to create uniform data across the country — something that’s sorely lacking.
In Pennsylvania, programs within the ICWC system receive state and federal funding, but they’re leaving additional federal dollars — dollars that can unlock meaningful innovation like what’s happening in Oklahoma and elsewhere — on the table. Providers in Pennsylvania can apply for a CCBHC designation (COMHAR notably did so), but it’s different from the “demonstration” models — which further adds to the confusing methods of data collection, versus a more unified, consistent approach that would happen if all states participated in the same program.
In October, a new Harris Poll, the 2022 CCBHC Impact Report, found that CCBHCs on average serve more than 900 more people per clinic than prior to CCBHC implementation, a 23 percent increase. CCBHCs offer access to services much faster than the national average wait time. CCBHCs provide access to certain forms of substance use disorder (SUD) treatment at vastly higher rates than non-CCBHCs. And CCBHCs’ direct crisis care capabilities continue to divert people from emergency departments and jails.
The possibility of returning to the CCBHC demonstration model, Edley says, is always on the agenda during meetings with legislators in Harrisburg, and will continue to be a big push as a new administration prepares to take office.
“I go to meetings around the country all the time where people talk about how amazing the CCBHC demonstration model is and how it’s going to more states and more clinics and how this is the national movement to be a part of. And then I think about how Pennsylvania is the exception,” Edley says. “Why do we always have to be so special?”