Five years ago, I developed a cough that would not go away. Further medical investigation found that I had developed a fibrotic lung condition called interstitial lung disease. Although I was assured it would get better with medication, my condition became progressively worse over the next three years. I was on continuous oxygen and could not even walk 20 feet without resting. I had to give up my career that I loved as an orthopedic surgeon.
I was listed for a lung transplant as my only remaining option. My condition was deteriorating rapidly and the procedure was needed as soon as possible. I received my first lung transplant — a single right lung — on May 19, 2022.
What a relief … I was saved!!! Or so I thought. I was free of external oxygen. With the help of physical therapy, I was able to walk further — eventually walking nearly two miles. I could even walk upstairs without stopping due to exhaustion! I was happy with the progress.
A setback
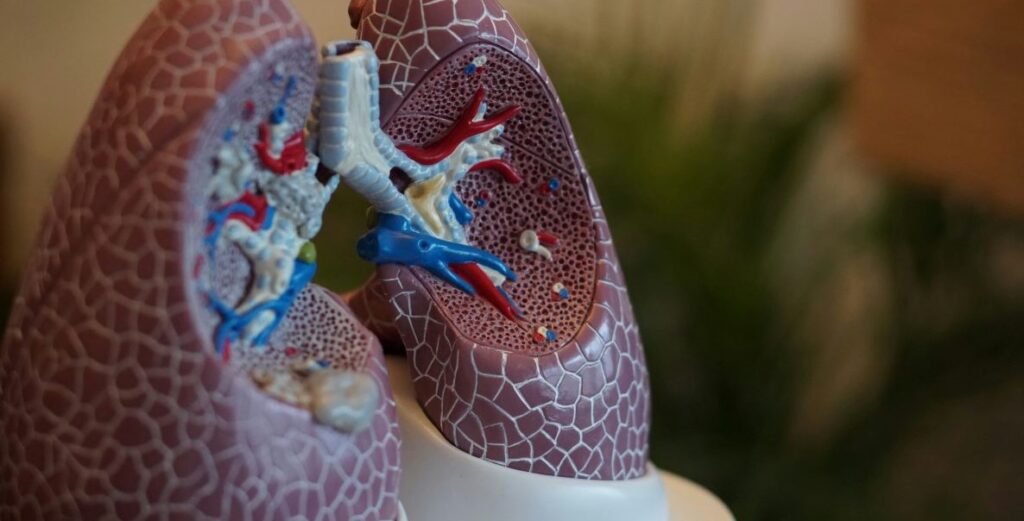
Then it started. I developed a series of serious infections requiring multiple hospital admissions and extensive intravenous antibiotics for over six months. Multiple bronchoscopies (where a camera is placed down the throat into the lungs to look around and clean them out), also showed severe stenosis (or narrowing) of my airway where the new lung had been attached, as well as progressive scarring to the transplanted lung itself, making it difficult for me to move air in and out of my lungs.
The physician team was amazing, trying everything in their armamentarium to get me to improve. The medication side effects were severe, yet despite curing the infections, the damage to the lung had become too severe and irreversible. I was undergoing frequent pulmonary function testing (PFTs) which showed my function to be like that of an 80-year-old chronic smoker with COPD, yet I have never even taken a single puff of a cigarette!
The donors and their families are the real heroes of this story.
After a final bronchoscopy in July 2023 — 14 months after my initial transplant — I was given the news that the transplant had prematurely failed. To survive, I would require a redo lung transplant. This would require removing both my lungs (the transplanted one and the old scarred one they had left in my chest) to have the best chance of a successful result.
Despite the scariness of this news, I was excited to have the opportunity to live again. At this point, I am essentially housebound without the breath to walk even short distances. I have to take rests walking up the one flight of stairs to our bedroom — something I restricted myself to doing once a day. But, with the support of my amazing wife, my family and my faith, I am still excited by the opportunity to live again.
The waiting begins … and continues
This is where my current story starts. To undergo a lung transplant you need to have a matching donor with your same blood type, and approximately the same height and size. [Editor’s note: gender, ethnic background do not need to match.] There is a scoring system that favors the sickest patients receiving a lung before the more chronic, like myself. This makes sense on one level, but published research statistics have demonstrated that healthier and less deconditioned recipients have significantly better outcomes following a redo transplant of the lung.
I asked my team how long I might have to wait before a set of lungs would be available. I do not blame them for the vagueness of their answer, but it was hard to take: “You could get the call tomorrow, or it could take as long as a year or more.” Very little information was shared regarding statistics and likelihood of how long the wait would be.
Fortunately, much of this information is online, so I will share some stats with you. According to the latest data from the Scientific Registry of Transplant Recipients (SRTR), over 3,100 candidates are added to the lung transplant waiting list every year (and increasing annually). Of those, 46 percent are between ages 50 and 64, and 72 percent are between height 5’2” and 5’11” (I personally fit into these statistics), with taller patients getting transplants sooner. Blood types follow normal population statistics.
On the donor side, there were 2,631 deceased donors gifting their lungs for transplantation in 2021. Unfortunately, 8 percent of these (210 sets of lungs) could not be used due to damage to the organs, leaving 2,421 sets of lungs available. In 2021, 2,569 lucky patients received these lifesaving gifts and underwent a lung transplant, with 20 percent receiving a single lung allowing more transplants than donors available. That still left a severe deficit in the number of lungs available compared to the number of patients on the list waiting for a transplant. While 63 percent of patients waited less than 90 days for their transplant, 15 percent had to wait more than a year for their transplant, while others are still waiting.
The donors and their families are the real heroes of this story. While still young and healthy they mark on their driver’s license their willingness to donate their organs in the event of an untimely death. Then their families, at a time of great personal tragedy, think of others in gifting their loved one’s organs to save a stranger’s life. There are no words to express how special this gift is and how much thanks are owed to these superstars. But bottom line: Unless more of the population becomes organ donors, the worse the deficit will become.
I am amongst those still waiting. It has been 172 days and counting. That’s about six months. My “go bag” is packed, as is my wife’s, who will accompany me to the hospital. I have had “the talk” with my children and wife about if something goes wrong during the procedure. I have had my affairs in order for some time. Every time the phone rings — my heart stops, but to date, all have been unrelated callers.
So how does this feel? Depressing! Nothing prepared me for how hard it has been. Every day I feel I am getting worse — able to do less. I’m hanging on a fraying string and don’t know how much longer I can hold on. Yet, every day I go on. I wait with my phone in my hand for the call. May it come soon.
Steven Raikin, a former orthopedic surgeon at Thomas Jefferson University Hospital, lives in Montgomery County.
The Citizen welcomes guest commentary from community members who represent that it is their own work and their own opinion based on true facts that they know firsthand.